treatment of pressure ulcers
- related: Dermatology
- tags: #dermatology
Regular Management
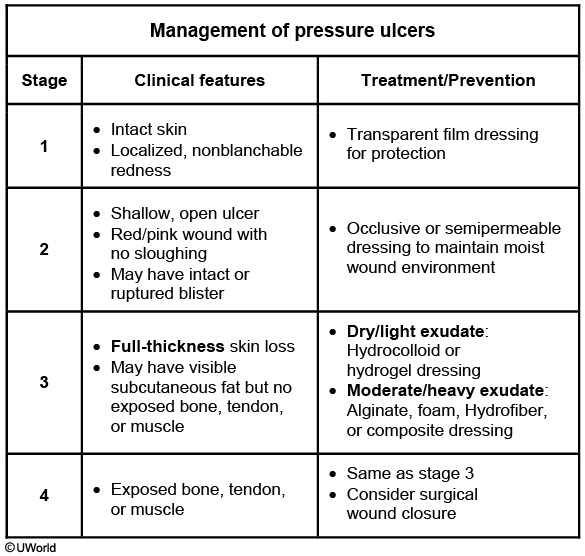
This patient has a stage 3 pressure ulcer. All patients with such ulcers require pressure relief measures, including scheduled patient turning, and optimized nutritional status. Wound fluids contain tissue growth factors that facilitate reepithelialization and wound healing, but excess fluid may cause wound maceration. Therefore, it is important to provide a balanced moist wound environment while keeping the surrounding skin dry.
Absorbent dressings are appropriate for wounds with significant exudate as they can remove the excess exudate while maintaining a moist environment. This patient has a dry wound without exudate or evidence of infection and would benefit from a semipermeable dressing (eg, hydrocolloid, hydrogel) to promote a moist wound environment. Dressings should generally be changed every 1-2 days.
Occlusive dressings (eg, DuoDerm) can be used on stage 2 ulcers, but they are not recommended for full-thickness (stage 3, 4, or unstageable) ulcers. These dressings can create an anaerobic environment that promotes infection, prevents inspection, and causes deep fistula formation.
Wet-to-dry and wet-to-wet saline gauze dressings are frequently used to aid debridement of wounds with extensive exudate. However, gauze dressings are labor intensive and do not reliably maintain a moist wound environment.
Vacuum-assisted closure (VAC) devices continuously or intermittently apply negative pressure to the wound surface. This promotes tissue remodeling and increased blood flow and decreases tissue edema. VAC has been found effective for diabetic foot wounds but has uncertain benefit for pressure ulcers.[1]
Nonhealing

This patient has a stage III pressure ulcer, defined as full-thickness skin loss with possible visible subcutaneous fat. Initial management of pressure ulcers includes local wound care, repositioning of the patient to relieve pressure, pain control, and nutritional support. Patients who do not improve with conservative therapy require evaluation for signs of infection (eg, erythema, purulent drainage, tenderness, fluctuance). Patients without signs of infection can be treated with a 2-week course of topical antibiotics. [2]
Patients with signs of local infection can be treated with topical antibiotics, whereas patients with cellulitis (eg, erythema, warmth, swelling over involved area) or sepsis/bacteremia require systemic antibiotics. All patients with signs of infection should undergo debridement. Surgical debridement removes necrotic tissue and accumulated debris, which helps to decrease bacterial load and stimulate wound epithelialization. This patient has necrotic tissue with signs of local infection (grayish slough, foul-smelling drainage) without cellulitis; therefore, she should receive debridement and topical antibiotics (Choice E). If there is no improvement, she should undergo tissue biopsy, MRI of the sacrum, and possibly bone biopsy to exclude osteomyelitis (Choice C). [3]
(Choice B) Pressure ulcers cause a chronic catabolic state and require adequate nutrition for proper wound healing. However, this patient first needs nutritional assessment (eg, protein/caloric intake, serum albumin and/or prealbumin) before considering enteral nutritional supplementation.
Occlusive dressings may help with wound healing by preventing contamination and absorbing excess fluid to prevent wound maceration. However, they are usually done after debridement and control of local infection.